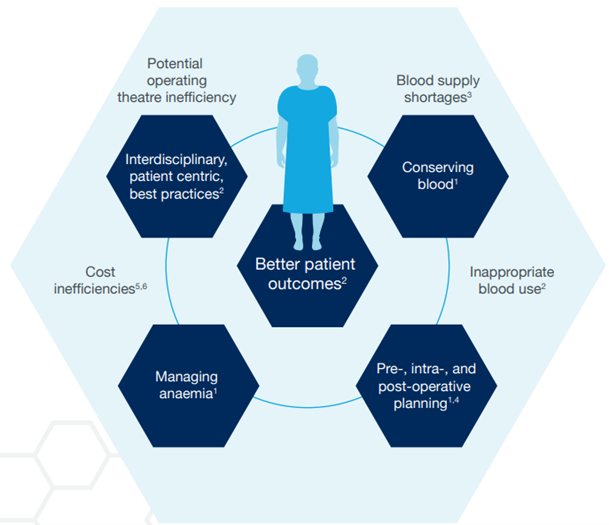
Reducing the demand through blood conservation can help manage supplies more effectively; this takes many forms and may occur in both medical and surgical settings.4 The cost of allogeneic red blood cells has increased over time.5 Transfusion reactions account for almost 35% of the cost of allogeneic RBC transfusions1, and RBC transfusions have been shown to be independently associated with significantly higher hospital costs.6
Financial implications of transfusions support the implementation of PBM and efforts to reduce the rate of RBC transfusions.6 By focussing on measures for the avoidance of transfusion and reducing the inappropriate use of blood, implementation of PBM improves patient outcomes and helps to reduce healthcare costs.3
Ongoing concerns over current and possible future blood shortages have resulted in increased efforts to manage the blood supply more efficiently, by increasing the supply and reducing the demand for blood.7 Allogeneic blood transfusion, whilst needed in certain cases, is impacted by reduced blood donations8, carries potential cost implications9 and is not without risks compared to autologous blood transfusion.10 There is an increased awareness of the risks of thrombosis with blood transfusions.
| | Allogeneic (donor) blood transfusion |
|---|
 | Risks | Cost implications | Availability |
 | - Wrong blood incidents/human error - Transmission of infection - Higher morbidity and mortality - Immunosuppression/ autoimmunisation: more difficult match second time around | - High costs that are rising - Length of stay - Costs associated with transfusion reactions - Potential waste if surgery rescheduled | - Affected by blood shortages - Blood supply is limited and can expire |