Organisms. Despite the meticulous qualification process and safety checks in place, blood transfusions are still associated with potential risks, such as infections, fever, allergic reactions, transfusion-related acute lung injury (TRALI), transfusion-associated circulatory overload, venous and arterial thrombotic events, and iron overload, which can lead to increased morbidity and mortality in critically ill patients. 8,9 The risk of these occurring increases with the number of RBC units transfused, and may be greater with blood that has been stored longer as ageing RBCS are inducers of oxidative stress, which can lead to inflammation and lung disease damage.10
Infectious
Organisms such as bacteria, viruses, prions, and parasites can be transmitted through blood transfusions. Infectious complications from blood transfusions have decreased over the past years due to improved donor questionnaires and sophisticated blood screening.11In particular virus screening as improved with pathogens such as hepatitis and human immunodeficiency virus (HIV) routinely screened for before in potential blood donors. As the presence of bacteria is not routinely tested in eligible blood donor, transmission of bacteria through blood transfusions is much more frequent than viruses and bacteria are the leading cause of death in transfusion transmitted infections.12
Non-Infectious
Non-infectious serious hazards of transfusion (NISHOTs) are currently the most frequent forms of complications of transfusion. NISHOTs include everything from well-described and categorized transfusion reactions (hemolytic, febrile, septic, and allergic/urticarial/anaphylactic) to lesser known complications.11
Non-infectious complications can be classified as acute and delayed reactions based on time of occurrence and further subclassified as immune or non-immune. Additionally, RBC and platelet transfusions is associated with increased risk of venous and arterial thrombotic events, however the causality of this relationship is still to be determined.8
Table 1. Non-infectious complications.| | Acute Reaction (<24 hours) | Delayed Reaction (>24 hours) |
|---|
 | Immune-mediated reactions | Non-immune mediated reactions | Immune-mediated reactions | Non-immune mediated reactions |
 | Acute hemolytic transfusion reaction (AHTR) | Air embolism | Delayed hemolytic transfusion reaction (DHTR) | Iron overload |
 | Febrile nonhemolytic transfusion reaction (FNHTR) | Transfusion-associated circulatory overload (TACO) | Alloimmunization - To HLA antigens - To platelet antigens - To red cell antigens | Allergic reactions |
 | Allergic reactions | Non-immune hemolysis | Transfusion-related immunomodulation (TRIM) | |
 | Anaphylactic reactions | | Transfusion-associated graft versus host disease (TA-GVHD) | |
 | Transfusion-related acute lung injury (TRALI) | | Post-transfusion purpura (PTP) | |
Post-transfusion alloimmunisation is the main complication observed after one or more RBCs concentrates transfusions, also sometimes observed after platelet concentrates transfusions.13 Alloimmunization refers to an immune response to foreign antigens from another human and may be followed by clinical complications.
Increased incidence of postoperative infection and risk of cancer recurrence in patients who have received allogeneic blood transfusions suggests that transfusions might be associated with clinically significant immunomodulatory effects (TRIM).14
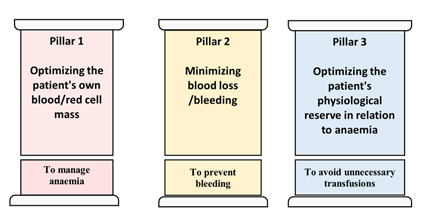
Given these risks, it is therefore advisable to minimize allogenic RBC transfusion where possible. Once potential strategy for this during surgical bleeding is by cell salvage.